Who We Serve
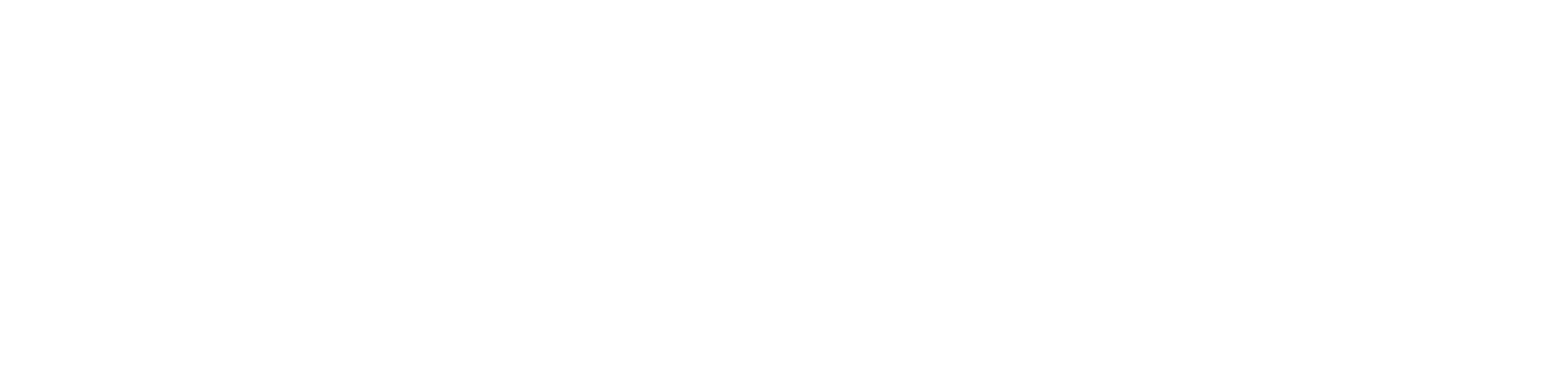
Agentic Analytics for Modern Health Plans
SemantIQ lets payer teams ask questions and get answers instantly from years of claims history, without waiting weeks for custom analyses or needing complex prompts. The platform shows how each answer is derived, so teams can trust and validate the results. A shared semantic layer ensures all teams are working from the same definitions and evidence, reducing friction and building confidence in the results. Together, this helps teams quickly understand utilization trends, network coverage, provider performance, and population risk - enabling smarter decision-making for benefits, care management, provider incentives, and total cost of care.

Overview of Interface
Designed with an intuitive experience users love.
An intuitive interface means can quickly understand how to perform talks without the need for training or guidance.
Team Collabration
Designed Around Your Vision
An intuitive interface means can quickly understand how to perform talks without the need for training or guidance.
Monetization
Unlock sustainable growth and powerful monetization
An intuitive interface means can quickly understand how to perform talks without the need for training or guidance.

Get in Touch
Ready to drive speed to insight with built-in compliance and governance? Send us a message and a member of our team will be in touch!